Little is known, however, about the GHRH population between birth and puberty. Notably, in the reports in which adult sex differences have been identified, there is broad agreement that they are not influenced by adult gonadectomy ( 25, 29, 34– 36), whereas neonatal gonadectomy reduces GHRH cell numbers in the adult male arcuate nucleus to levels indistinguishable from those seen in normal females ( 35). For example, in rodents there are reports that GHRH neuronal number, mRNA, or peptide levels in the male arcuate nucleus may be greater than or the same as that in females ( 24– 34). In particular, the precise sexually dimorphic nature of the adult GHRH population and the determining factors remain controversial and poorly characterized.
Our previous findings therefore clearly demonstrate that the period between birth and puberty represents a time of dramatic change in the neuroregulation of the GH axis, at least in the somatostatin pathway, which presages the adult patterns of GH release, but this remains a relatively unexplored area. Moreover, we have reported that sexual differentiation of this somatostatin pathway actively continues beyond the critical period for differentiation of the brain but before the pubertal rise in gonadal steroids ( 16– 18), even though circulating GH levels remain low, nonpulsatile, and similar in males and females during this period ( 10– 12). To that end we characterized the organizational and activational influences of gonadal factors in newborn and adult rats, respectively, on PeN somatostatin neurons ( 16– 19), which accord with the ability of sex hormones to imprint and activate sex dimorphisms in GH secretion ( 20– 23). It is therefore important that we have a clear understanding of the ontogeny and sexual differentiation of the GH neuroregulatory pathways. These sex-specific GH secretory profiles greatly influence mammalian GH physiology throughout life as they trigger sex- and tissue-specific patterns of gene expression and signal transduction mechanisms that impact on normal male/female patterns of growth and metabolism ( 6, 14, 15). In concert with the inhibitory somatostatin neurons in the periventricular nucleus (PeN), they drive a pulsatile pattern of GH secretion ( 2– 9), which becomes markedly sexually dimorphic at puberty ( 10– 13). The GHRH neurons of the hypothalamic arcuate nucleus provide the major stimulus for GH biosynthesis and release from the adult anterior pituitary gland ( 1). This information adds to our knowledge of processes that underpin the emergence of sex-specific GH secretory dynamics and hence biological activity of this pleiotropic hormone. They also provide the first demonstration of emergent sex-specific GHRH architecture, which may signal the onset of sex-dependent regulation of activity reported for adult GHRH-eGFP neurons, and its differential regulation by gonadal factors in males and females. These findings establish a novel ontogenetic profile for GHRH neurons and suggest previously undiscovered roles for peripubertal gonadal factors in establishing population size in both sexes.
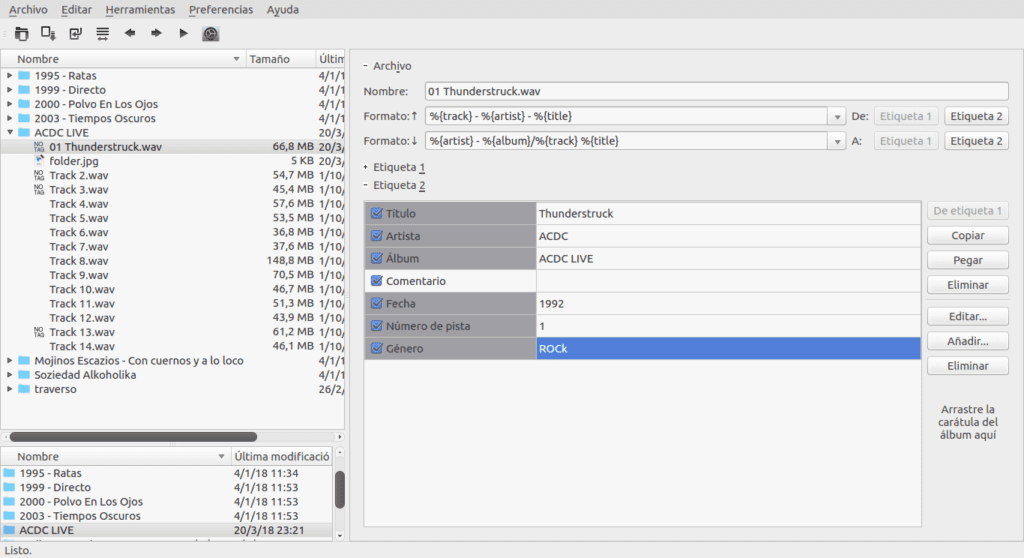
Intriguingly, prepubertal gonadectomy (P28), unlike adult gonadectomy, caused a dramatic 40% loss of GHRH cells in both sexes in adulthood and a significant (30%) increase in processes emanating from cell bodies only in females. Conversely, we identified the emergence of male-dominant sex differences in the number of processes extended per GHRH perikarya across puberty. Thereafter (P20, P30, P60, P365) there was a significant trend for numbers to decrease in males and increase in females, such that sex differences were, surprisingly, absent in young and late adulthood. Using the GHRH-enhanced green fluorescent protein (eGFP) transgenic mouse, in which eGFP provides a strong surrogate signal for identifying GHRH neurons, we showed that numbers in the male arcuate nucleus were double those seen in females at x postnatal day (P)1 and P10, during which time numbers increased 2- to 3-fold.
GH secretion and growth rates are developmentally regulated and sexually dimorphic, but the neuroregulatory mechanisms between birth and puberty are unclear.

 0 kommentar(er)
0 kommentar(er)
